- Understanding Disability Benefits for Herniated Disc
- What is a Herniated Disc?
- Explaining the Condition and its Impact on Daily Life
- Qualifying for Disability Benefits
- Evaluating the Severity of the Herniated Disc
- Question-answer:
- What is a herniated disc?
- Can a herniated disc cause disability?
- What are the symptoms of a herniated disc?
- How is a herniated disc diagnosed?
- What are the treatment options for a herniated disc?
- What is a herniated disc?
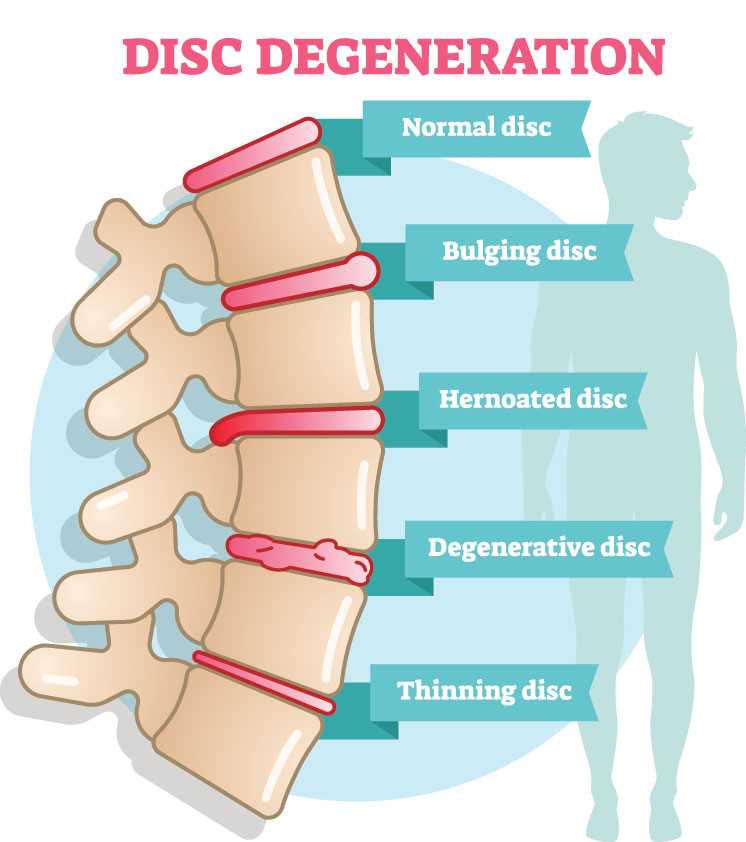
A herniated disc, also known as a slipped or ruptured disc, is a common condition that can cause severe pain and disability. It occurs when the soft cushion-like material between the vertebrae in the spine bulges or ruptures, putting pressure on the nerves. This can result in pain, numbness, and weakness in the affected area, as well as radiating pain down the arms or legs.
Living with a herniated disc can be challenging, as it can limit your ability to perform everyday tasks and activities. If you are unable to work due to the pain and limitations caused by your herniated disc, you may be wondering if you can qualify for disability benefits.
The answer to this question depends on several factors, including the severity of your condition, the impact it has on your ability to work, and the specific requirements of the disability program you are applying for. In general, to qualify for disability benefits for a herniated disc, you will need to provide medical evidence that supports your claim and shows that your condition meets the criteria outlined by the Social Security Administration (SSA) or other disability programs.
It is important to note that simply having a herniated disc does not automatically qualify you for disability benefits. The SSA evaluates disability claims based on the severity of the condition and its impact on your ability to work. They will consider factors such as the intensity and frequency of your pain, the limitations it imposes on your daily activities, and the effectiveness of any treatments you have undergone.
If you are considering applying for disability benefits for a herniated disc, it is advisable to consult with a qualified disability attorney or advocate who can guide you through the application process and help you gather the necessary medical evidence to support your claim. They can also help you understand the specific requirements of the disability program you are applying for and increase your chances of a successful outcome.
Understanding Disability Benefits for Herniated Disc
When it comes to herniated discs, understanding the disability benefits available can be crucial for individuals who are unable to work due to the condition. Herniated discs can cause severe pain and limit a person’s ability to perform daily activities, making it difficult to maintain employment.
Disability benefits for herniated discs are typically provided through the Social Security Administration (SSA). The SSA offers two types of disability programs: Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI).
SSDI is available to individuals who have worked and paid into the Social Security system, earning enough credits to qualify for benefits. To be eligible for SSDI benefits, the herniated disc must meet the SSA’s criteria for disability, which includes a determination that the condition prevents the individual from engaging in substantial gainful activity (SGA).
SSI, on the other hand, is a needs-based program that provides benefits to individuals with limited income and resources. To qualify for SSI benefits, the individual must meet the SSA’s income and asset limits, as well as the criteria for disability.
When applying for disability benefits for a herniated disc, it is important to provide medical evidence that supports the severity of the condition and its impact on daily life. This may include medical records, imaging studies, and statements from healthcare providers.
The SSA will evaluate the severity of the herniated disc by considering factors such as the individual’s ability to walk, stand, sit, lift, and perform other physical activities. They will also assess the individual’s ability to perform work-related tasks, such as following instructions, maintaining concentration, and interacting with others.
If the SSA determines that the herniated disc meets their criteria for disability, the individual may be eligible to receive monthly disability benefits. The amount of benefits will depend on factors such as the individual’s work history and earnings.
What is a Herniated Disc?
A herniated disc, also known as a slipped or ruptured disc, is a condition that affects the spine. The spine is made up of a series of bones called vertebrae, and between each vertebra is a disc that acts as a cushion. These discs are made up of a tough outer layer called the annulus fibrosus and a soft gel-like center called the nucleus pulposus.
When a disc herniates, it means that the gel-like center has pushed through a crack or tear in the outer layer. This can happen due to age-related wear and tear, injury, or excessive strain on the spine. When the gel-like center pushes out, it can put pressure on nearby nerves, causing pain, numbness, and weakness in the affected area.
A herniated disc can occur in any part of the spine, but it is most common in the lower back (lumbar spine) and the neck (cervical spine). The symptoms of a herniated disc can vary depending on the location and severity of the herniation. Some people may experience mild discomfort, while others may have severe pain that affects their daily activities.
It is important to note that not all herniated discs cause symptoms. In fact, many people may have a herniated disc without even realizing it. However, if the herniated disc is causing significant pain or affecting your ability to function, it may be necessary to seek medical treatment.
Treatment for a herniated disc can range from conservative measures such as rest, physical therapy, and pain medication, to more invasive options like surgery. The appropriate treatment will depend on the severity of the herniation and the individual’s specific symptoms and needs.
Explaining the Condition and its Impact on Daily Life
A herniated disc, also known as a slipped or ruptured disc, occurs when the soft cushion-like material between the vertebrae in the spine pushes out through a crack in the outer layer. This condition can cause severe pain and discomfort, as well as a range of other symptoms.
When a herniated disc occurs, it can put pressure on nearby nerves, leading to pain, numbness, and weakness in the affected area. The location of the herniated disc will determine which parts of the body are affected. For example, if the herniation is in the lower back, it may cause pain and weakness in the legs and feet.
The impact of a herniated disc on daily life can be significant. The pain and discomfort can make it difficult to perform everyday tasks, such as sitting, standing, walking, or lifting objects. Simple activities like getting dressed or driving a car can become challenging and painful.
In addition to physical limitations, a herniated disc can also have a significant impact on a person’s mental and emotional well-being. Chronic pain can lead to feelings of frustration, depression, and anxiety. The constant pain and limitations can also affect a person’s ability to work, socialize, and enjoy their usual activities.
It is important to note that the severity of the impact will vary from person to person. Some individuals may experience mild symptoms and be able to manage their condition with conservative treatments, while others may have more severe symptoms that require more intensive medical intervention.
If you are experiencing symptoms of a herniated disc and it is affecting your daily life, it is important to seek medical attention. A healthcare professional can provide a proper diagnosis and recommend appropriate treatment options to help manage your symptoms and improve your quality of life.
Qualifying for Disability Benefits
When it comes to qualifying for disability benefits for a herniated disc, there are certain criteria that need to be met. The severity of the herniated disc and its impact on your daily life will be evaluated to determine if you are eligible for benefits.
The first step in the evaluation process is to provide medical evidence of your herniated disc. This can include medical records, imaging tests such as MRI or CT scans, and doctor’s reports. The medical evidence should clearly show the diagnosis of a herniated disc and the extent of the condition.
Next, the severity of your herniated disc will be assessed. The Social Security Administration (SSA) uses a set of guidelines called the Blue Book to evaluate the severity of various medical conditions, including herniated discs. The Blue Book lists specific criteria that must be met in order to qualify for disability benefits.
For a herniated disc to meet the criteria in the Blue Book, it must result in one of the following:
- Nerve root compression
- Spinal arachnoiditis
- Lumbar spinal stenosis
- Motor loss
If your herniated disc does not meet the criteria in the Blue Book, you may still be eligible for benefits if it can be shown that your condition is equivalent in severity to a listed impairment. This is known as a medical-vocational allowance.
In addition to meeting the medical criteria, you must also meet the non-medical requirements for disability benefits. This includes having enough work credits to qualify for Social Security Disability Insurance (SSDI) or having a low income and limited resources to qualify for Supplemental Security Income (SSI).
Overall, qualifying for disability benefits for a herniated disc can be a complex process. It is important to gather all necessary medical evidence and consult with a disability attorney to ensure that you meet the criteria and have the best chance of receiving benefits.
Evaluating the Severity of the Herniated Disc
When determining eligibility for disability benefits, the severity of the herniated disc is a crucial factor. The Social Security Administration (SSA) evaluates the severity based on medical evidence provided by the applicant.
The SSA will consider the following factors when evaluating the severity of a herniated disc:
- Objective medical evidence: The SSA will review medical records, imaging tests, and other diagnostic reports to assess the severity of the herniated disc. This evidence should clearly demonstrate the presence of a herniated disc and its impact on the individual’s ability to perform daily activities.
- Treatment history: The SSA will evaluate the applicant’s treatment history, including medications, physical therapy, surgeries, and other interventions. The effectiveness of the treatment and its impact on the individual’s functional abilities will be considered.
- Functional limitations: The SSA will assess the functional limitations caused by the herniated disc. This includes limitations in standing, walking, sitting, lifting, bending, and other physical activities. The severity and duration of these limitations will be taken into account.
- Residual functional capacity (RFC): The SSA will determine the applicant’s RFC, which is their ability to perform work-related activities despite their impairments. The RFC assessment considers the individual’s physical abilities, such as lifting, carrying, and sitting, as well as any mental limitations.
- Medical opinions: The SSA may also consider medical opinions from healthcare professionals, including treating physicians and medical experts. These opinions can provide additional insight into the severity of the herniated disc and its impact on the individual’s ability to work.
It is important for applicants to provide comprehensive and detailed medical evidence to support their claim for disability benefits. This includes medical records, imaging reports, treatment history, and any relevant medical opinions. The more evidence provided, the stronger the case for disability benefits.
Overall, the severity of the herniated disc is a critical factor in determining eligibility for disability benefits. By understanding the evaluation process and providing thorough medical evidence, individuals with a severe herniated disc can increase their chances of receiving the financial support they need.
Question-answer:
What is a herniated disc?
A herniated disc occurs when the soft cushion-like material between the vertebrae in the spine ruptures or bulges out. This can put pressure on nearby nerves, causing pain, numbness, and weakness.
Can a herniated disc cause disability?
Yes, a herniated disc can cause disability. The severity of the symptoms and the impact on a person’s ability to work or perform daily activities will determine if they are eligible for disability benefits.
What are the symptoms of a herniated disc?
The symptoms of a herniated disc can vary depending on the location and severity of the herniation. Common symptoms include back pain, leg pain, numbness or tingling in the affected area, muscle weakness, and difficulty walking or standing for long periods of time.
How is a herniated disc diagnosed?
A herniated disc is typically diagnosed through a combination of medical history, physical examination, and imaging tests such as X-rays, MRI, or CT scans. These tests can help determine the location and severity of the herniation.
What are the treatment options for a herniated disc?
Treatment options for a herniated disc may include rest, physical therapy, pain medication, epidural steroid injections, and in severe cases, surgery. The specific treatment plan will depend on the individual’s symptoms and the extent of the herniation.
What is a herniated disc?
A herniated disc occurs when the soft cushion-like material between the vertebrae in the spine ruptures or bulges out. This can put pressure on nearby nerves, causing pain, numbness, and weakness.